Authors: LCDR Glen Cook, MD, USN, MC; LT Charles Mitschow, MD, USN, MC. Translated with AI.
The polygraph and other emerging technologies are used to aid in interrogations and employee screenings, but examiners and physicians should be aware that results are susceptible to inaccuracies in subjects with autonomic disorders and can be confounded by multiple medications.
The United States Department of Defense (DoD) and law enforcement agencies across the country use the polygraph as an aid in security screening processes and interrogations. It is assumed that an interviewee will have a visceral response when attempting to deceive the interviewer, and that this response can be detected by measuring the change in vital signs between questions. By using vital signs as an indirect measurement of stress induced by deception, the polygraph machine can provide a false positive or negative result if a patient has an inherited or acquired condition affecting the autonomic nervous system (ANS).
A variety of diseases, from alcohol use disorder to rheumatoid arthritis, can affect the ANS (Autonomic Nervous System). Additionally, a multitude of commonly prescribed medications can affect the ANS. Although still in their early stages, deception detection techniques using functional magnetic resonance imaging (fMRI) and electroencephalogram (EEG) avoid these issues. Dysautonomias may be an underestimated cause of error in the interpretation of polygraph results. Polygraph examiners and DoD agencies should be aware of the potential for these disorders to interfere with the interpretation of results. In the near future, other modalities that do not measure autonomic variables could be used to avoid these difficulties.
POLYGRAPH

Throughout history, humans have shown an interest in techniques and devices capable of discerning truth from lies. Even in ancient times, it was known that the act of lying had physiological effects. In ancient Israel, if a woman accused of adultery developed a swollen abdomen after drinking “bitter waters,” she was considered guilty of the crime. In ancient China, those accused of fraud were forced to keep dry rice in their mouth; if the spat-out rice was dry, the suspect was declared guilty. We now know that catecholamines, particularly epinephrine, secreted during moments of stress, cause smooth muscle relaxation, leading to a reduction in intestinal motility and dry mouth. However, most methods before the modern era were based more on superstition and chance than on any solid physiological premise.
When people are asked to discern between truth and falsehood based on their own perceptions, they correctly identify lies as false only 47% of the time and truth as non-deceptive about 61% of the time. In short, without assistance, we are very poor lie detectors. Therefore, there has been great interest in technology that can aid in lie detection. With the improvement of technology and understanding of human physiology, interest in lie detection was renewed. Since it was known that vital signs such as blood pressure (BP), heart rate, and respiration could be affected by the stressful situation caused by deception, quantifying and measuring those responses in an effort to detect lies became a goal. In 1881, Italian criminologist Cesare Lombroso invented a glove that, when worn by a suspect, measured their BP. Changes in BP were also the target variable of the systolic blood pressure lie detection test invented by William M. Marston, PhD, in 1915. Marston also experimented with measurements of other variables, such as muscle tension. In 1921, John Larson invented the first modern polygraph machine.
Procedures The modern polygraph is based on these techniques. A standard polygraph measures breathing, heart rate, blood pressure (BP), and sudomotor function (sweating). Breathing is measured by strain gauges attached around the chest and abdomen that respond to chest expansion during inhalation. BP and pulse can be measured through various means, including pulse measurement on the finger or the sphygmomanometer.
Sweating is measured by the electrical conductance of the skin. Human sweat contains a variety of cations and anions, mainly sodium and chloride, but also potassium, bicarbonate, and lactate. The presence of these electrolytes alters the electrical conduction on the skin surface when sweat is released.
The Supreme Court of the United States has ruled that individual jurisdictions can decide whether or not to admit polygraph tests in court, and the United States Court of Appeals for the Eleventh Circuit has established that polygraph results are only admissible if both parties agree and are notified well in advance. Currently, New Mexico is the only state that allows polygraph results to be used as evidence without a pre-trial agreement; all other states require such an agreement or prohibit the results from being used as evidence.
Although rarely used in federal and state courts as evidence, polygraphy is commonly used during investigations and in the hiring process of government agencies. The Department of Defense (DoD) Directive 5210.48 and Instruction 5210.91 allow DoD investigative organizations (e.g., Naval Criminal Investigative Service, National Security Agency, U.S. Army Criminal Investigation Command) to use the polygraph as an aid during investigations related to suspicion of involvement with foreign intelligence, terrorism against the U.S., mishandling of classified documents, and other serious violations.
The Role of the Physician in Polygraph Evaluation It may be rare for a physician to be asked to provide information on an individual’s medical condition or related medication use and its effect on polygraph results. However, in such cases, the physician must remember the primary fiduciary duty to the patient. Medical conditions cannot be disclosed without the patient’s consent, except in very specific situations (e.g., Commanding Officer’s Inquiry, Tarasoff Duty to Protect, etc.). It is the responsibility of the polygraph examiner to be aware of potential confounding factors in a particular examination.
Physicians may have a responsibility, when in administrative or supervisory positions, to advise security officials and others regarding the fitness for certain tasks of candidates with whom there is no doctor-patient relationship. This may include an individual’s ability to undergo a polygraph examination and the validity of such results. However, when a doctor-patient relationship is involved, care must be taken to ensure that the patient understands that the relationship is protected by both professional standards and law, and that information will not be shared without the patient’s authorization (apart from those rare exceptions provided by law). Often, a direct explanation to the patient about their medical condition and the possible effects of any medication on polygraph results will be sufficient, allowing the patient to inform the polygraph examiner as much as deemed necessary.
Dangers of Polygraphy
Polygraphy presupposes that the subject will have a consistent and measurable physiological response when attempting to deceive the interviewer. Changes in blood pressure (BP), heart rate, respirations, and sweating detected by polygraphy and interpreted by the examiner are controlled by the autonomic nervous system (ANS) (Table 1). There are several diseases known to cause autonomic dysfunction (dysautonomia). Small fiber autonomic neuropathies often result in loss of sweating and changes in heart rate and BP variation and can arise from many underlying conditions. Synucleinopathies, such as Parkinson’s disease, alter cardiovascular reflexes.
Table 1: Physiological Measurements Made by Polygraphy
Breathing: Measured by strain gauges around the chest and abdomen, which respond to the expansion of the chest during inhalation.
Heart Rate: Can be measured using various methods, including pulse measurement on the finger or using a sphygmomanometer.
Blood Pressure (BP): Assessed through different means, potentially including a sphygmomanometer or similar devices to gauge fluctuations during the examination.
Sudomotor Function (Sweating): Determined by the electrical conductance of the skin, which changes due to the presence of sweat containing electrolytes like sodium, chloride, potassium, bicarbonate, and lactate.
Even diseases not commonly recognized for having a predominant clinical impact on ANS function may demonstrate a measurable physiological effect. For example, about 60% of patients with rheumatoid arthritis will have attenuated cardiac vagal baroreceptor responses and heart rate variability. ANS dysfunction is also a common sequel of alcoholism. Patients with diabetes mellitus often have an elevated resting heart rate and low heart rate variability due to deregulated β-adrenergic activity. The impact of reduced baroreceptor response and decreased heart rate variability could affect a polygraph interpreter’s ability to discern responses using heart rate. Individuals with ANS dysfunction causing attenuated physiological responses might have inconclusive polygraph results or, potentially worse, false negatives due to lack of variation between control and target questions.
To our knowledge, no studies have been conducted on the validity of polygraphy in patients with any form of dysautonomia. Furthermore, a 2011 Department of Defense (DoD) polygraph program process and compliance study specifically recommended that “adjudicators would benefit from training in the capabilities and limitations of polygraphy.” Although specific requirements vary from one program to another, all programs accredited by the American Polygraph Association provide training in physiology, psychology, and standardization of test results.
Many commonly prescribed medications have effects on the ANS that could affect the results of a polygraph examination (Table 2). For instance, β-blockers reduce the activation of β-adrenergic receptors in cardiac muscle and blood vessels, decreasing heart rate, heart rate variability, cardiac contractility, and blood pressure (BP). This class of medications is prescribed for a variety of conditions, including congestive heart failure, hypertension, panic disorder, and post-traumatic stress disorder. Thus, a patient taking β-blockers would have an attenuated physiological response to stress and a higher probability of obtaining an inconclusive or false negative polygraph examination.
Table 2: Medications Affecting the ANS (Autonomic Nervous System)

β-Blockers
Effect on ANS: Decrease heart rate, heart rate variability, cardiac contractility, and blood pressure by inhibiting β-adrenergic receptors.
Common Uses: Hypertension, heart failure, anxiety disorders, arrhythmias.
Alpha-Blockers
Effect on ANS: Lower blood pressure by inhibiting α-adrenergic receptors, which reduces vascular resistance.
Common Uses: Hypertension, benign prostatic hyperplasia.
Anticholinergics
Effect on ANS: Block acetylcholine at muscarinic receptors, reducing parasympathetic activity.
Common Uses: Overactive bladder, COPD, Parkinson’s disease symptoms.
Cholinesterase Inhibitors
Effect on ANS: Increase acetylcholine concentration at synaptic clefts, enhancing parasympathetic signals.
Common Uses: Alzheimer’s disease, myasthenia gravis.
Central Nervous System Stimulants
Effect on ANS: Increase heart rate and blood pressure, enhance alertness by increasing catecholamine activity.
Common Uses: ADHD, narcolepsy.
SSRIs (Selective Serotonin Reuptake Inhibitors)
Effect on ANS: Can cause changes in heart rate and blood pressure; mechanisms involving serotonin modulation of the ANS.
Common Uses: Depression, anxiety disorders.
Tricyclic Antidepressants
Effect on ANS: Can cause orthostatic hypotension, tachycardia, and other autonomic disturbances due to anticholinergic effects.
Common Uses: Depression, neuropathic pain.
Calcium Channel Blockers
Effect on ANS: Decrease blood pressure and reduce heart rate by blocking calcium channels in the heart and blood vessels.
Common Uses: Hypertension, angina, arrhythmias.
Diuretics
Effect on ANS: Can indirectly affect autonomic responses through volume changes and electrolyte imbalances.
Common Uses: Hypertension, heart failure, edema.
MAO Inhibitors (Monoamine Oxidase Inhibitors)
Effect on ANS: Can increase blood pressure and affect autonomic responses by inhibiting the breakdown of monoamine neurotransmitters.
Common Uses: Depression, Parkinson’s disease.
Each of these medication classes can influence the outcomes of a polygraph test by altering the physiological responses that the test seeks to measure. Therefore, it’s crucial for examiners and medical professionals to be aware of a subject’s medication history when interpreting polygraph results.
Common Medications, Their Effects on the ANS, and Physiological Effects
β-Blockers
Examples: Propranolol, Atenolol, Metoprolol
Effect on the ANS: Block noradrenergic β-1 and/or β-2 receptors
Physiological Effects: Reduction of heart rate, reduction of blood pressure
α-1 Blockers
Examples: Tamsulosin, Prazosin
Effect on the ANS: Block noradrenergic α-1 and/or α-2 receptors
Physiological Effects: Reduction of blood pressure, may increase heart rate
Tricyclic Antidepressants
Examples: Amitriptyline, Nortriptyline
Effect on the ANS: Block acetylcholine receptors
Physiological Effects: Reduction of sweating, increase in heart rate
Antihistamines
Examples: Diphenhydramine
Effect on the ANS: Block acetylcholine receptors
Physiological Effects: Reduction of sweating, increase in heart rate
Carbonic Anhydrase Inhibitor
Examples: Acetazolamide
Effect on the ANS: Inhibition of carbonic anhydrase
Physiological Effects: Reduction in sweating response
α-2 Agonists
Examples: Clonidine, Guanfacine
Effect on the ANS: Bind and activate α-2 receptors
Physiological Effects: Reduction of blood pressure, may increase heart rate
Some over-the-counter medications also have effects on autonomic function. Sympathomimetics like pseudoephedrine or antihistamines with anticholinergic activity like diphenhydramine can increase both heart rate and blood pressure. Of the 10 most prescribed medications in 2016, 5 have direct effects on the ANS or the variables measured by the polygraph machine. An exhaustive list of the effects of medications on autonomic function is beyond the scope of this article.
A medication that can affect the results of a polygraph study and is of particular interest to the Department of Defense (DoD) and the military is mefloquine. Mefloquine is an antimalarial drug that has been used by military personnel deployed in malaria-endemic regions. In murine models, mefloquine has been shown to alter autonomic and respiratory control in the central nervous system. The neuropsychiatric adverse effects of mefloquine are well documented and can last years after drug exposure. Therefore, mefloquine could affect the results of a polygraph test both through direct toxic effects on the ANS and by causing anxiety and depression, potentially affecting the subject’s response to interrogation.
ALTERNATIVE MODALITIES
Given the inherent dangers of using external physiological measures for lie detection, additional modalities that avoid measuring responses governed by the ANS have been sought. Indeed, the integration and combination of more comprehensive modalities have come to be termed forensic credibility assessment.
Functional Magnetic Resonance Imaging (fMRI)
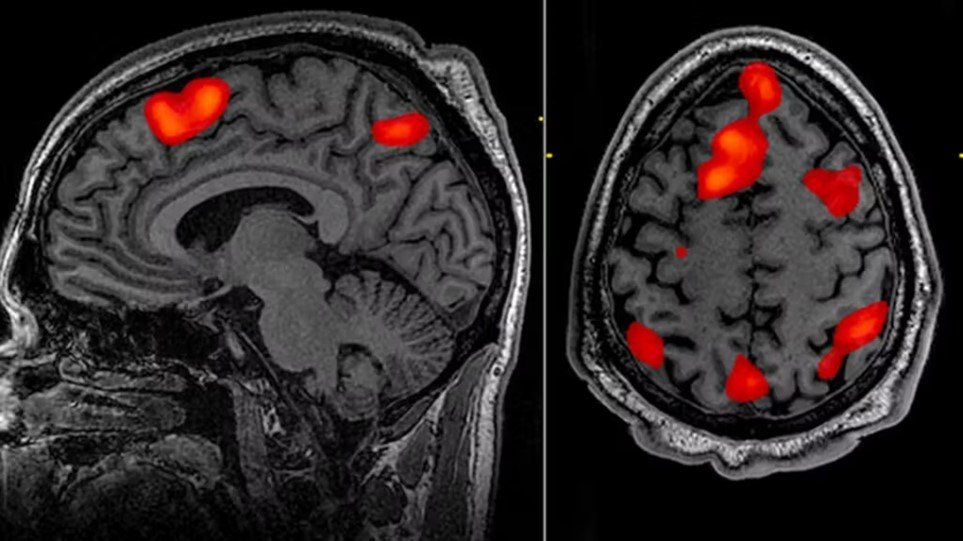
Since 1991, researchers began using fMRI to observe real-time changes in perfusion in areas of the cerebral cortex between moments of rest and mental stimulation. This modality provides a non-invasive technique to visualize which specific parts of the brain are stimulated during activity. When someone is actively deceiving, the dorsolateral prefrontal cortex exhibits increased perfusion compared to when the individual is telling the truth. Since fMRI involves imaging for the evaluation of the central nervous system, it avoids potential inaccuracies seen in some subjects with autonomic irregularities. In fact, fMRI may offer superior sensitivity and specificity for lie detection compared to conventional polygraphy.
Significant limitations to the use of fMRI include the need for costly specialized equipment and trained personnel to operate the MRI. Agencies using polygraph examinations may not be willing to make such an investment. Additionally, subjects with metallic foreign bodies or incompatible medical implants cannot undergo the MRI procedure. Finally, bioethical and legal concerns have been raised that measuring brain activity during interrogation could endanger “cognitive liberty” and might even be considered an unreasonable search and seizure under the Fourth Amendment of the U.S. Constitution. However, like polygraphy, fMRI can only measure the difference in cerebral perfusion in 2 states. The idea of fMRI as “mind reading” is largely a misconception.
Functional magnetic resonance imaging (fMRI) represents an alternative modality in deception detection that moves away from reliance on physiological measures controlled by the autonomic nervous system (ANS). Instead of measuring peripheral physiological responses such as blood pressure, heart rate, breathing, or skin conductance, fMRI focuses on direct neuronal activity, providing high-resolution images of changes in cerebral blood flow related to neuronal activity.
When a person is engaged in the act of lying or performing cognitively demanding tasks (such as recalling a lie or fabricating a story), certain brain areas show increased activity. fMRI can detect these changes in brain activity by measuring variations in the signal due to changes in blood oxygen levels, a phenomenon known as the Blood Oxygen Level Dependent (BOLD) effect.
Studies using fMRI to detect deception have identified several brain regions that are more frequently activated during dishonesty, including the prefrontal cortex, areas involved in inhibitory control, and the cingulate cortex, associated with conflict resolution. These areas are critical for decision-making processes, suggesting that lying involves greater cognitive effort than telling the truth.
fMRI has several advantages over traditional lie detection methods, including:
Improved Specificity and Sensitivity: Ability to more accurately identify the brain regions involved in deception.
Less Vulnerable to Manipulation: Since it measures brain activity directly, subjects are less likely to be able to consciously manipulate their responses to falsify results.
Potential to Reveal the Cognitive Nature of Deception: Offers insights into the cognitive and emotional processes involved in the act of lying.
However, there are also challenges and limitations in using fMRI for lie detection, such as:
Cost and Accessibility: fMRI scanners are expensive and not widely available.
Complex Interpretation: Interpreting fMRI data requires specialized expertise and can be complex.
Ethical and Privacy Concerns: The idea of “mind reading” raises significant ethical and privacy concerns about how this information might be used or misinterpreted.
In summary, although fMRI offers a promising approach to deception detection, ongoing research is necessary to overcome its current limitations and to establish clear guidelines for its ethical and effective use in forensic and security contexts.
Electroencephalography

Electroencephalography (EEG) is a technique used to record electrical activity of the brain. It involves the placement of electrodes on the scalp to detect and record patterns of electrical activity generated by brain cells. EEG is widely used in both clinical and research settings for a variety of purposes, including the diagnosis of neurological conditions such as epilepsy and sleep disorders, as well as for studying brain function and cognition.
EEG is particularly valued for its high temporal resolution, which allows it to track changes in brain activity on the scale of milliseconds. This makes it an excellent tool for studying the dynamics of mental processes, including attention, perception, and cognitive responses to stimuli.
In the context of deception detection, EEG has been explored as a potential method to identify neural correlates of lying or truth-telling. Research has focused on identifying specific brainwave patterns or event-related potentials (ERPs) that are associated with deceptive responses. For example, certain ERP components, such as the P300 wave, have been studied for their potential to indicate recognition of familiar or relevant information that a person might be trying to conceal.
The advantages of using EEG for lie detection include its non-invasiveness, relatively low cost compared to imaging techniques like fMRI, and its ability to provide real-time monitoring of brain activity. However, there are also challenges and limitations associated with EEG-based lie detection, including:
Variability in Individual Responses: There can be significant variation in how individuals’ brains respond to lying, making it difficult to establish universal markers of deception.
Susceptibility to Countermeasures: Individuals may be able to use cognitive or physical techniques to alter their brain activity and potentially evade detection.
Complexity of Deception: Lying is a complex cognitive and emotional process that may not be fully captured by simple EEG measures.
Ethical and Legal Considerations: Similar to fMRI, the use of EEG for lie detection raises questions about privacy, consent, and the potential for misuse.
Despite these challenges, EEG remains an area of active research in the field of deception detection, with ongoing efforts to refine methods and improve accuracy. As with any lie detection technology, the ethical and legal implications of its use must be carefully considered.
Various EEG modalities have garnered increasing interest for lie detection. In EEG, electrodes are used to measure the summation of a multitude of postsynaptic action potentials and the local voltage gradient they produce when cortical pyramidal neurons fire synchronously. These voltage gradients are detectable on the scalp’s surface. Shortly after the invention of EEG, it was observed that specific stimuli generated unique and predictable changes in EEG morphology. These event-related potentials (ERP) are detectable by scalp EEG shortly after the stimulus is administered.
ERPs can be elicited by a multitude of sensory stimuli, have a predictable and reproducible morphology, and are believed to be a psychophysiological correlate of mental processing of stimuli. The P300 is an ERP characterized by a positive change in voltage occurring 300 milliseconds after a stimulus. It is associated with the processing and categorization of the stimulus. Since deception is a complex cognitive process involving recognizing relevant stimuli and inventing false responses to them, it was theorized that detecting a P300 ERP during an interview with the patient would mean that the patient indeed recognizes the stimulus and is denying such knowledge. Early studies on the P300 had variable accuracy for lie detection, about 40% to 80%, depending on the study. Thus, the false negative rate would increase if subjects were instructed on countermeasures, such as increasing the significance of distractor data or counting backward in sevens. Later studies have found ways to minimize these issues, such as detecting a P900 ERP (a cortical potential at 900 milliseconds) that can be observed when subjects attempt countermeasures.
Another technique to increase accuracy in EEG-mediated lie detection is the measurement of the multifaceted electroencephalographic response (MER), which involves a more detailed analysis of multiple EEG electrode sites and how signaling changes over time using both visual comparison of multiple trials and bootstrap analysis. Specifically, the memory and encoding-related multifaceted electroencephalographic response (MERMER) using P300 along with an electrically negative pulse recorded in the frontal lobe and phase shifts in the global EEG had superior accuracy than P300 alone.
The benefits of EEG compared to fMRI include significant reductions in costs, space, and restrictions for use in some people (EEG is safe for virtually all patients, including those with metallic foreign bodies). However, like fMRI, EEG still requires trained personnel to operate and interpret. Additionally, it has yet to be tested outside of the laboratory.
CONCLUSION
The ability to detect deception is an important factor in determining security risk and adjudicating legal proceedings, but untrained individuals are surprisingly poor at discerning truth from lies. The polygraph has been used by law enforcement and governmental agencies for decades to assist in interrogations and in screening employees for security clearances and other types of access. However, results are vulnerable to inaccuracies in subjects with autonomic disorders and can be confounded by multiple medications. While emerging technologies like fMRI and EEG may allow for greater accuracy by circumventing SNA-based physiological outputs, both the polygraph examiner and the physician must be aware of the effect of autonomic dysfunction and medications affecting the SNA. This is particularly true in military medicine, as many patients within this population are subject to polygraph examinations.
Authors: LCDR Glen Cook, MD, USN, MC; LT Charles Mitschow, MD, USN, MC. Translation assisted by AI.

Recent Comments